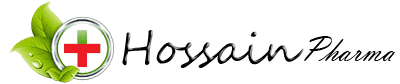
Windel Plus | Nebuliser Solution | 6 pcs
৳ 150.00
Brand Name: Windel Plus Nebuliser Solution
Generic: Salbutamol + Ipratropium
(2.5 mg+500 mcg)/3 ml
Manufacturer: Incepta Pharmaceuticals Ltd.
3 ml ampoule: ৳ 25.00 (3 x 6: ৳ 450.00)
Indications
Therapeutic Class
Description
Pharmacology
Ipratropium Bromide is quickly absorbed after inhalation. The systemic bioavailability following inhalation is estimated to be less than 10% of the dose. Renal excretion of Ipratropium Bromide is given as 46% of the dose after intravenous administration. The half-life of the terminal elimination phase is about 1.6 hours as determined after intravenous administration. Elimination half-life of drug and metabolites is 3.6 hours as determined after radio labelling. Ipratropium Bromide does not penetrate the blood brain barrier.
Salbutamoi Sulphate is rapidly and completely absorbed following administration either by inhaled or oral route. Peak plasma Salbutamoi concentrations are seen within three hours of administration and it is excreted unchanged in the urine after 24 hours. The elimination half-life is 4 hours. Salbutamoi will cross the blood brain barrier reaching concentrations amounting to about five percent of the plasma concentrations.
It has been shown that co-nebulisation of Ipratropium Bromide and Salbutamoi Sulphate does not potentiate the systemic absorption of either component and that therefore the additive activity of this solution is due to the combined local effect on the lung following inhalation.
Dosage
Salbutamol sulfate & Ipratropium bromide solution for inhalation in ampoule may be administered from a suitable nebulizer or an intermittent positive pressure ventilator.
- Adults (including elderly): Use one 3 ml ampoule in the nebulizer four times a day. Two additional treatments may be used per day, if needed.
- Children: Use and dose must be determined by doctor.
Patients should be advised to consult a doctor or the nearest hospital immediately in the case of acute or rapidly worsening dyspnoea if additional inhalations do not produce an adequate improvement.
Administration
Step 2: Squeeze the desired amount of the nebulizer solution into the nebulizer chamber.
Step 3: If dilution is needed follow the physician’s direction.
Interaction
The concurrent administration of other beta-mimetics, systemically absorbed anticholinergics and xanthine derivatives may increase the side effects.
Beta-agonist induced hypokalaemia may be increased by concomitant treatment with xanthine derivatives, glucocorticosteroids and diuretics. This should be taken into account particularly in patients with severe airway obstruction.
Hypokalaemia may result in an increased susceptibility to arrhythmias in patients receiving digoxin. It is recommended that serum potassium levels be monitored in such situations.
A potentially serious reduction in bronchodilator effect may occur during concurrent administration of beta-blockers.
Beta-adrenergic agonists should be administered with caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants, since the action of beta adrenergic agonists may be enhanced.
Inhalation of halogenated hydrocarbon anaesthetics such as halothane, trichloroethylene and enflurane may increase the susceptibility to the cardiovascular effects of beta-agonists.
Contraindications
Side Effects
In common with other beta-agonists containing products, side effects of this solution can include fine tremor of skeletal muscles and nervousness and less frequently tachycardia, dizziness, palpitations or headache, especially in hypersensitive patients.
Potentially serious hypokalaemia may result from prolonged and/or high dose beta2 agonist therapy.
As with use of other inhalation therapy, cough, local irritation and less commonly inhalation induced bronchospasm can occur. As with other beta-mimetics, nausea, vomiting, sweating, weakness and myalgia/muscle cramps may occur. In rare cases decrease in diastolic blood pressure, increase in systolic blood pressure, arrhythmias, particularly after higher doses, may occur.
In individual cases psychological alterations have been reported under inhalation therapy with beta-mimetics.
The most frequent non-respiratory anticholinergic related adverse events are dryness of mouth and dysphonia. There have been isolated reports of ocular complications (i.e. mydriasis, increased intraocular pressure, angle closure glaucoma, and eye pain) when aerosolised ipratropium bromide either alone or in combination with adrenergic beta2 agonist, has escaped into the eyes. Ocular side effects, gastrointestinal motility disturbances and urinary retention may occur in rare cases and are reversible.
Pregnancy & Lactation
Pregnancy category C. Animal studies with Salbutamoi Sulphate have demonstrated a teratogenic effect. It is not known whether this medication is harmful to the fetus. No evidence of abnormalities has been reported in women receiving albuterol during pregnancy. This solution should be used during pregnancy only if the potential benefit justifies. This solution should be used with caution before childbirth in view of Salbutamol’s inhibitory effects on uterine contractions.
Salbutamol Sulphate and Ipratropium Bromide are probably excreted in breast milk and their effects on neonates are not known. Although lipid-insoluble quaternary bases pass into breast milk, it is unlikely that this will happen to any extent especially when taken by inhalation. However, because many drugs are excreted in breast milk, caution should be exercised when This solution is administered to a nursing woman.
Precautions & Warnings
Overdose Effects
The effects of overdosage are expected to be primarily related to Salbutamol because acute overdosage with Ipratropium Bromide is unlikely as it is not well absorbed systemically after inhalation or oral administration.
Symptoms: Manifestations of overdosage with salbutamol may include tachycardia, anginal pain, hypertension, hypotension , palpitations, tremor, widening of the pulse pressure, arrhythmia and flushing.
Therapy: Administration of sedatives, tranquillisers; in severe cases, intensive therapy. Beta-receptor blockers, preferably beta1-selective, are suitable as specific antidotes; however, a possible increase in bronchial obstruction must be taken into account and the dose should be adjusted carefully in patients suffering from bronchial asthma.
Storage Conditions
| Generic Name | Salbutamol + Ipratropium |
|---|---|
| Size | 3 ml |
Only logged in customers who have purchased this product may leave a review.





Reviews
There are no reviews yet.